In Part 1 of this 2-part article, we took a look at the prevalence and impact of digital device use. Part 2 below discusses the clinical performance of DigitalBoost™ technology.
DigitalBoost™: Tackling lens discomfort and ocular tiredness with technology
Demonstrating CooperVision’s commitment to continuous innovation, CooperVision has introduced the optical design found in Biofinity Energys® contact lenses to the MyDay® family with the introduction of MyDay Energys® in March of 2023. Both products offer a wide prescription range, providing correction for 99.7% of prescriptions31.
As outlined above, maintaining comfortable lens wear in digital device users is crucial. Aquaform® Technology used in the comfilcon A material and common to all Biofinity® and MyDay® contact lenses, allows for naturally wettable silicone hydrogel materials without the need for surface treatment or wetting agents. In the matrix of long silicone chains, hydrogen bonds form to lock water molecules within the lens, for inherent wettability and a comfortable lens-wearing experience. This allows the lens to attract and retain moisture. The long chains mean that less silicone is needed, resulting in a material with balanced properties of water content, modulus, and oxygen transmissibility.
In addition to the comfort benefits of the Aquaform Technology, MyDay Energys® and Biofinity Energys® lenses feature the DigitalBoost™ lens design, which helps with eye tiredness caused by focusing on digital devices (Figure 1). Multiple front-surface aspheric curves distribute power evenly to simulate positive power across the entire optic zone, providing +0.3D of DigitalBoost so wearers can change focus from on-screen to off-screen and back with less effort. This eases accommodative burden and may help reduce ciliary stress32,**. Distance vision is not adversely impacted by the unique DigitalBoost design and fitting MyDay Energys® and Biofinity Energys® in practice is no different to fitting a standard, spherical, single vision, soft lens*.
Clinical performance of DigitalBoost™
- Close focusing stress in current contact lens wearers
Viewing digital devices requires long periods of close focusing, which, in turn, requires sustained contraction of the ciliary muscle. This effort contributes to the symptoms of ocular tiredness, termed ‘asthenopia’, as described above. Accommodative micro-fluctuations result from spasm of the ciliary muscle when viewing a near target, and manifest as tremors or a state of temporal ocular instability33, and are measured as changes in the refractive power of the eye over time.
So can the simple act of wearing a contact lens designed to alleviate eye tiredness associated with close focusing make a measurable difference to the amount of stress the ciliary muscle is subjected to? This was investigated in a recent study. Accommodative micro-fluctuations were measured for a standardized close reading task on an iPhone using controlled screen brightness and ambient lighting conditions. Sixty-eight adapted lens wearers completed twenty minutes of reading at a 25 cm viewing distance, using both a standard spherical contact lens (Biofinity®) and the DigitalBoost™ design (Biofinity Energys®)32.
The change in accommodative micro-fluctuations from before to after the reading task was statistically lower for Biofinity Energys® compared to the standard spherical lens (Figure 2). This suggests DigitalBoost™ reduced ciliary muscle stress for the reading task set in the study, and that this novel design may be useful for digital device users who are experiencing symptoms32**.
- The ocular benefits of fitting neophytes with Energys technology
Are contact lenses with DigitalBoost™ a suitable option for neophytes? If comfortable use of digital devices is potentially more challenging for lens wearers, how does this technology compare to staying in spectacles? Are there benefits patients receive by switching to contact lenses? Sixty-one spectacle wearers who regularly used digital devices were eligible for inclusion in a study to investigate these questions34. Thirty two were fit with Biofinity Energys with DigitalBoost™, and twenty nine continued over the two month study period with their up to date single vision spectacles. The impact of wearing contact lenses on quality of life was quantified using a validated questionnaire35, and symptoms of computer vision syndrome were also assessed.
Quality of life scores increased over the two-month period for the contact lens wearing group, driven mainly by improved performance for outdoor, fitness activities and use of non-prescription sunglasses. The spectacle group reported similar, unchanged, quality of life scores between baseline and two months. At two months, the difference in scores between the two groups was judged to be both statistically significantly different and clinically meaningful. The lens wearing group reported significant and positive responses towards contact lenses suggesting they were highly satisfied with their correction34. In fact, the clinical performance and visual acuity of Biofinity Energys® with DigitalBoost™ was comparable to single vision spectacles34, demonstrating how well neophytes adapted to a monthly replacement contact lens. There were no differences in symptoms of computer vision syndrome questionnaire results between groups. These are useful results to bear in mind when considering whether to recommend contact lenses to patients for the first time.
Tips for Eye Care Professionals
- Leveraging Contact Lenses with DigitalBoost™
Based on the available evidence, Biofinity Energys® and MyDay Energys® contact lenses with DigitalBoost™ is suitable both for patients new to contact lenses, and for existing wearers who may be experiencing suboptimal visual comfort with their current lenses when using digital devices. In practice, ECPs can question their patients on their use of digital devices, in order to gain an understanding of the range of screens used and the time spent per day viewing them. It should be remembered that the patient may not volunteer their experience when using devices, perhaps believing that some degree of ocular discomfort is inevitable. This makes it extremely important to be proactive and enquire about their ocular comfort when viewing computers, tablets and smartphones.
When recommending MyDay Energys® or Biofinity Energys®, communicate their features to patients: the combination of a widely used silicone hydrogel lens material with a unique optical design to help alleviate the symptoms of tiredness that can occur with prolonged digital device use. If feasible, enabling the patient to experience the lenses while using their usual devices may be useful for them to experience the visual benefit of the DigitalBoost™.
It is always important to provide good education on the safe wear and care of contact lenses. New wearers should be supported with time to practice handling techniques and given access to information for their use at home to help remember the steps in their daily wear and care routine. Contact lens aftercare provides a regular opportunity to check the habits of existing wearers and correct any bad habits that have crept in. Practicing compliant lens wear not only minimizes the chances of an adverse event such as microbial keratitis36,37 or corneal infiltrative events38, but also helps to maximize comfortable wear time36.
Helping to alleviate digital device use symptoms in all patients
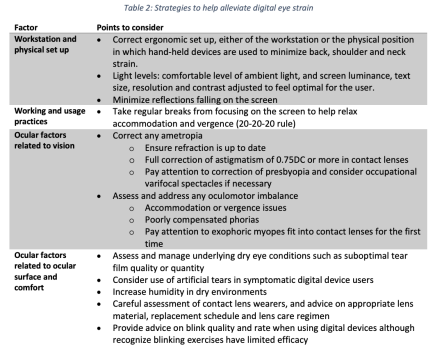
Beyond specific contact lens-related advice, there are a number of other tips ECPs can share with patients to help them manage any symptoms they may be experiencing (Table 2). Remember the nature of digital device use symptoms is often multifactorial, which results in an holistic approach being recommended to help address the condition1. Strategies to relieve, or better still, to prevent, symptoms have been covered in a number of reviews1-3. The ergonomic set up when using digital devices should be considered, and this necessarily varies depending on the type of device being used. Incorrect set up or poor posture can result in back, shoulder and neck strain7,43. Ambient light should be set to a comfortable level, and screen luminance, text size, resolution and contrast adjusted to feel optimal for the user. It can feel more comfortable to minimize any reflections falling on the screen, however evidence for the use of anti-glare filters remaining equivocal1. Refocusing on far objects has been found to be more effective than taking breaks from viewing devices alone44. The 20-20-20 rule is widely shared in the literature, which encompasses taking a twenty second break every twenty minutes to view something at least twenty feet away. Although it has been pointed out that this ‘rule’ has not been validated or the subject of peer review45, it does form common sense advice to help relax accommodation and vergence to limit the amount of asthenopia experienced.
Ocular factors to address in cases of digital device use symptoms include ensuring the refraction is up to date, that any presbyopia is appropriately corrected, and in soft contact lenses, any astigmatism of 0.75DC or more is corrected46,47. ‘Occupational’ varifocals or prescriptions specific to device viewing distances may be helpful. The use of spectral filters, such as blue light filters, is growing in popularity, however a recent systematic review suggested more research is required to confirm their efficacy48. Oculomotor balance should be assessed, addressing any accommodative or vergence issues present. Take care to assess convergence and how well compensated any exophoria is in myopes newly fit with contact lenses; they lose the effect of base in help in their spectacles when wearing their contact lenses.
Underlying dry eye conditions such as suboptimal tear film quality or quantity should be investigated and managed. The combination of altered blink rate, increased number of incomplete blinks16,19. and time spent in air conditioned environments all add to the chance of ocular surface dryness. The integrity of the ocular surface should be carefully checked with diagnostic dyes such as fluorescein, and any aqueous or evaporative tear film issues present managed. Symptomatic screen users may also benefit from using artificial tears. Increasing humidity in dry environments can help to improve ocular comfort49. Blinking exercises can be prescribed, or on-screen blinking prompts may be used, however both strategies have limited effect in reducing eye strain1,50. Remember too that contact lens wearers are at increased risk of ocular discomfort and digital lifestyle symptoms21,23,51, and beyond considerations of accurate correction of refraction, and appropriate lens material, replacement schedule and care system, the use of suitable lubricating drops may also be beneficial in this group52.
Conclusions
Rather than asking patients if they use digital devices, perhaps the more useful route in today’s world is to ask how many types of screens they use regularly and for how long each day. Do not let patients assume digital lifestyle symptoms and fatigue are expected side effects of sustained screen viewing. Proactive questioning and appropriate refractive and ocular surface assessment will help elicit issues, providing greater opportunity for the ECP to intervene with advice and management strategies.
Wearing a contact lens designed for these tasks adds an additional challenge to the tear film and increases the chance of ocular discomfort and fatigue. Results shared here illustrate that beyond general advice for the management of digital eye strain, relief from accommodative stress is possible via use of a lens designed to help alleviate ocular tiredness**. MyDay Energys® and Biofinity Energys® have been designed to meet the visual demands of patients’ modern lifestyles and may benefit both existing and new contact lens wearers who routinely use digital devices.
References
*CVI Data on file 2016. Prospective, multi-center, subject-masked, bilateral, one month dispensing study in USA with Biofinity Energys in existing Biofinity sphere wearers. N=52. At dispensing and after one month of wear.
** Based on a statistically significant difference of the mean change in Accommodative Microfluctuations and when compared to Biofinity sphere after reading on an iPhone for 20 minutes.
1. Coles-Brennan C, Sulley A, Young G. Management of digital eye strain. Clinical & experimental optometry. 2019;102(1):18-29.
2. Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ open ophthalmology. 2018;3(1):e000146.
3. Jones L, Ng A, Thompson B. Continuing Education: Keeping Up with Ocular Fatigue in the Digital Era. Contact Lens Spectrum. 2016;31:3-10.
4. Pew Research Center. Technology Device Ownership: 2015. https://www.pewresearch.org/internet/2015/10/29/technology-device-ownership-2015/. Accessed 02 Sep 2020.
5. Pew Research Center. Mobile Fact Sheet. 2019. https://www.pewresearch.org/internet/fact-sheet/mobile/. Accessed 02 Sep 2020.
6. YouGov. European eye fatigue study. April 2016.
7. The Vision Council. Eyes Overexposed: The digital device dilemma; 2016 Digital Eye Strain Report. https://visionimpactinstitute.org/wp-content/uploads/2016/03/2016EyeStrain_Report_WEB.pdf. Accessed 02 Sep 2020.
8. Meeker M. Internet Trends 2017 https://www.kleinerperkins.com/perspectives/internet-trends-report-2017/. Accessed 02 Sep 2020.
9. The Common Sense Census: Media Use by Tweens and Teens, 2019. https://www.commonsensemedia.org/research/the-common-sense-census-media-use-by-tweens-and-teens-2019. Accessed 02 Sep 2020.
10. Livingston G. Americans 60 and older are spending more time in front of their screens than a decade ago. 2019. https://www.pewresearch.org/fact-tank/2019/06/18/americans-60-and-older-are-spending-more-time-in-front-of-their-screens-than-a-decade-ago. Accessed 02 Sep 2020.
11. Coronavirus productivity data: How the pandemic is changing the way we use digital devices, apps, and tools. 2020. https://blog.rescuetime.com/coronavirus-device-usage-statistics/. Accessed 02 Sep 2020.
12. 29% of US Consumers will Increase Long-term Use of Digital Channels Because of COVID-19 Pandemic. 2020. https://www.prnewswire.com/news-releases/29-of-us-consumers-will-increase-long-term-use-of-digital-channels-because-of-covid-19-pandemic-301058495.html. Accessed 02 Sep 2020.
13. Hall L, Brennan-Coles C. More screen time = more digital eye strain. Contact Lens Spectrum. June 2015;30:38-40.
14. Sheedy JE, Hayes JN, Engle J. Is all asthenopia the same? Optometry and vision science. 2003;80(11):732-739.
15. Jaiswal S, Asper L, Long J, Lee A, Harrison K, Golebiowski B. Ocular and visual discomfort associated with smartphones, tablets and computers: what we do and do not know. Clinical & experimental optometry. 2019;102(5):463-477.
16. Portello JK, Rosenfield M, Chu CA. Blink rate, incomplete blinks and computer vision syndrome. Optometry and vision science. 2013;90(5):482-487.
17. Patel S, Henderson R, Bradley L, Galloway B, Hunter L. Effect of visual display unit use on blink rate and tear stability. Optometry and vision science. 1991;68(11):888-892.
18. Schlote T, Kadner G, Freudenthaler N. Marked reduction and distinct patterns of eye blinking in patients with moderately dry eyes during video display terminal use. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2004;242(4):306-312.
19. Chu CA, Rosenfield M, Portello JK. Blink patterns: reading from a computer screen versus hard copy. Optometry and vision science. 2014;91(3):297-302.
20. Survey Reveals Parents Drastically Underestimate the Time Kids Spend on Electronic Devices. 2014. https://www.prnewswire.com/news-releases/survey-reveals-parents-drastically-underestimate-the-time-kids-spend-on-electronic-devices-268088521.html. Accessed 02 Sep 2020.
21. Gonzalez-Meijome JM, Parafita MA, Yebra-Pimentel E, Almeida JB. Symptoms in a population of contact lens and noncontact lens wearers under different environmental conditions. Optometry and vision science. 2007;84(4):296-302.
22. Uchino M, Schaumberg DA, Dogru M, et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology. 2008;115(11):1982-1988.
23. Tauste A, Ronda E, Molina MJ, Segui M. Effect of contact lens use on Computer Vision Syndrome. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians. 2016;36(2):112-119.
24. Alabdulkader B. Effect of digital device use during COVID-19 on digital eye strain. Clinical & experimental optometry. 2020. In press
25. Moshirfar M, West WB, Marx DP. Face Mask-Associated Ocular Irritation and Dryness. Ophthalmology and Therapy. 2020;9(3):397-400.
26. Jones L. Why face masks can make eyes feel dry, and what you can do about it. Aug 2020. https://theconversation.com/why-face-masks-can-make-eyes-feel-dry-and-what-you-can-do-about-it-143261. Accessed 02 Sep 2020.
27. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye & contact lens. 2013;39(1):93-99.
28. Dumbleton K, Caffery B, Dogru M, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Subcommittee on Epidemiology. Investigative ophthalmology & visual science. 2013;54(11):TFOS20-36.
29. Meyer D, Huenink S, Rickert P, Kollbaum P, Chamberlain P. Symptoms associated with eye fatigue in soft contact lens wearers. American Academy of Optometry Meeting; 2015; New Orleans.
30. CVI data on File 2020. Based on prescription options available across all soft lenses in sphere, toric, multifocal and toric multifocal, SiH and hydrogel, stock and made-to-order from 4 main manufacturers in UK, Germany, Italy and France. Cosmetic & Photochromatic CLs not included. Multiple base curve variants not included.
31. CVI data on file 2020. Rx coverage database; 14-70 years. Across sphere, toric and multifocal prescriptions.
32. Kajita M, Muraoka T, Orsborn G. Changes in accommodative micro-fluctuations after wearing contact lenses of different optical designs. Contact lens & anterior eye. 2020;43(5):493-496.
33. Campbell FW, Robson JG, Westheimer G. Fluctuations of accommodation under steady viewing conditions. The Journal of physiology. 1959;145(3):579-594.
34. Smith S, Morgan P, Orsborn G, Vega J, Maldonado-Codina C. Subjective Acceptance and Quality of Life with users of Comfilcon A Silicone Hydrogel Soft Contact Lenses in a Multiple Aspheric Curve Lens Design. Optometry and vision science. 2020;97(E-abstract):200028
35. Pesudovs K, Garamendi E, Elliott DB. The Quality of Life Impact of Refractive Correction (QIRC) Questionnaire: development and validation. Optometry and vision science. 2004;81(10):769-777.
36. Stapleton F, Keay L, Edwards K, et al. The Incidence of Contact Lens-Related Microbial Keratitis in Australia. Ophthalmology. 2008;115(10):1655-1662.
37. Dart JKG, Radford CF, Minassian D, Verma S, Stapleton F. Risk Factors for Microbial Keratitis with Contemporary Contact Lenses. A Case-Control Study. Ophthalmology. 2008;115(10):1647-1654.e1643.
38. Steele KR, Szczotka-Flynn L. Epidemiology of contact lens-induced infiltrates: an updated review. Clinical & experimental optometry. 2017;100(5):473-481.
39. Jones L, Walsh K, Willcox M, Morgan P, Nichols J. The COVID-19 pandemic: Important considerations for contact lens practitioners. Contact lens & anterior eye. 2020;43(3):196-203.
40. Arshad M, Carnt N, Tan J, Stapleton F. Compliance behaviour change in contact lens wearers: a randomised controlled trial. Eye (Lond). 2020: https://pubmed.ncbi.nlm.nih.gov/32546749/.
41. Arshad M, Carnt N, Tan J, Ekkeshis I, Stapleton F. Water Exposure and the Risk of Contact Lens-Related Disease. Cornea. 2019;38(6):791-797.
42. Lakkis C, George MA, Sulley A. COVID-19 and contact lenses: hygeine and compliance. In. Optician. September ed2020:20-29.
43. Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014;25:277-279.
44. Reddy SC, Low CK, Lim YP, Low LL, Mardina F, Nursaleha MP. Computer vision syndrome: a study of knowledge and practices in university students. Nepal J Ophthalmol. 2013;5(2):161-168.
45. Chou B. Deconstructing the 20-20-20 Rule for digital eye strain. 2018. https://www.optometrytimes.com/view/deconstructing-20-20-20-rule-digital-eye-strain. Accessed 02 Sep 2020.
46. Rosenfield M, Hue JE, Huang RR, Bababekova Y. The effects of induced oblique astigmatism on symptoms and reading performance while viewing a computer screen. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians. 2012;32(2):142-148.
47. Wiggins NP, Daum KM. Visual discomfort and astigmatic refractive errors in VDT use. Journal of the American Optometric Association. 1991;62(9):680-684.
48. Lawrenson JG, Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: a systematic review of the literature. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians. 2017;37(6):644-654.
49. Abusharha AA, Pearce EI. The effect of low humidity on the human tear film. Cornea. 2013;32(4):429-434.
50. Rosenfield M, Portello JK. Letter to the Editor: Computer Vision Syndrome and Blink Rate. Current eye research. 2016;41(4):577-578.
51. Ranasinghe P, Wathurapatha WS, Perera YS, et al. Computer vision syndrome among computer office workers in a developing country: an evaluation of prevalence and risk factors. BMC Res Notes. 2016;9:150.
52. Guillon M, Maissa C, Pouliquen P, Delval L. Effect of povidone 2% preservative-free eyedrops on contact lens wearers with computer visual syndrome: pilot study. Eye & contact lens. 2004;30(1):34-39.







