In the first part of this article, we reviewed the deeper emotional benefits around how contact lens wearers feel, and how eye care professionals can use that understanding to increase proactive recommendation. This second part will look at data on a new vision-related challenge for many, namely the issue of spectacle fogging when wearing a face mask, along with the opportunities for dual wear of both spectacles and contact lenses.
A new reason to try contact lenses
In response to the coronavirus pandemic, the wearing of face masks has become common place in 2020 and looks set to continue in 2021. Multi-national surveys of more than 8,000 consumers found more than 8 out of 10 spectacle wearers have experienced their spectacle lenses fogging up when wearing a mask (Figure 1).17,18 Nearly one in three (30%) have removed their spectacles and risked not seeing clearly to help cope with the issue, and 21% have worn their mask incorrectly, for example not covering their nose.18 Very few people had sought advice from their ECP (2%),18 yet in a European-based survey, 86% of people agreed they would be interested in finding out more about solutions to the issue.17
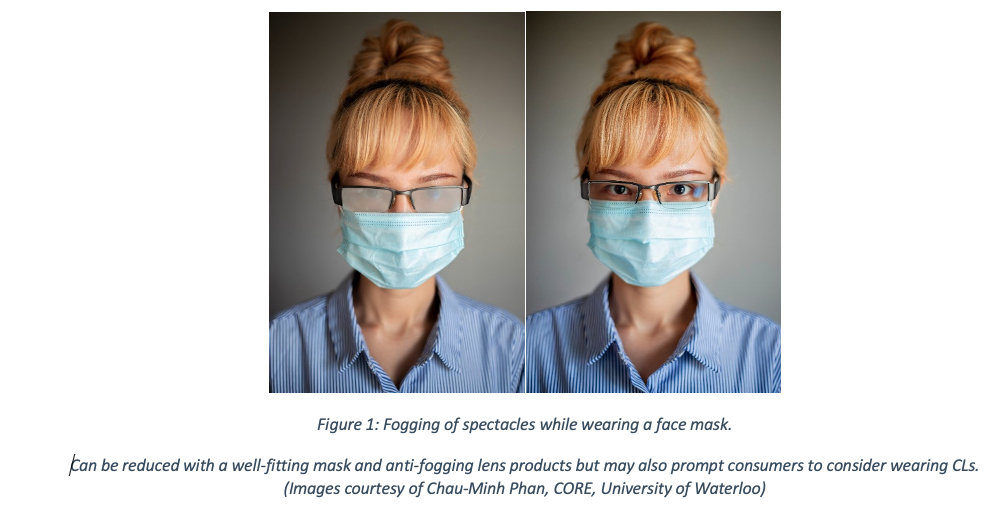
There is much the ECP can do to be proactive in this situation. First providing information on minimising spectacle fogging, at both routine appointments and in-patient email and website communications. Improving the fit of the mask and using anti-fogging lens wipes and sprays can help to some degree. However, for many people the more convenient solution is to consider CL wear, a suggestion the ECP can make with confidence knowing that 63% of consumers would consider CLs when wearing a mask.17 This may be particularly relevant for those required to wear face masks for long periods in the day. This not only includes healthcare workers using personal protective equipment (PPE), but also people working indoors in-service industries and office buildings where mask wearing may be mandated. In the current climate – and given the reticence of patients to speak up and ask their practitioner about it - ECPs have an important role to check that their patients are able to see clearly and comfortably when wearing face masks. An action that is expected by the majority of patients, with three-quarters expecting their ECP to tell them about all available eyecare options that could avoid their spectacles fogging up when wearing a mask.17
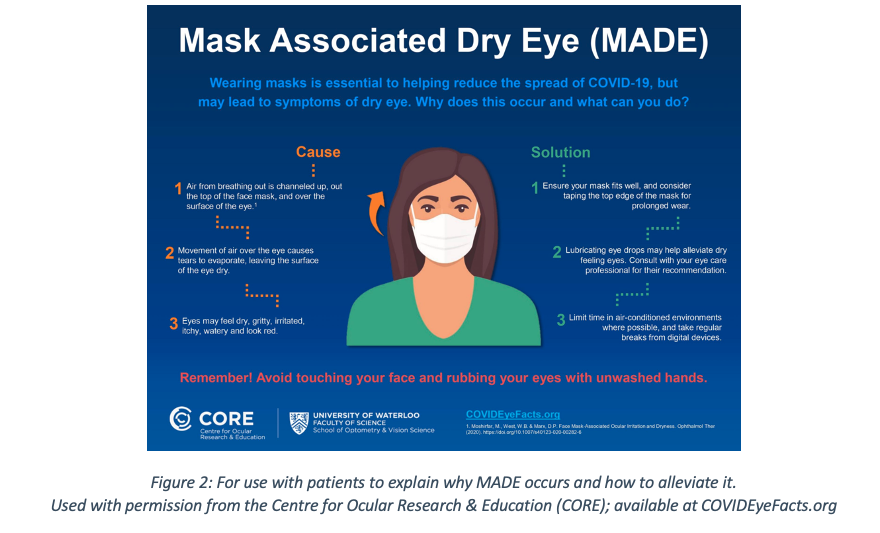
Related to this, and relevant for both spectacle and CL wearers is the need to proactively ask about ocular comfort when the mask is worn. In the same way loose fitting masks result in exhaled air fogging up spectacle lenses, the upward movement of air can also cause increased tear film evaporation and lead to ocular dryness.19,20 Remember here too that the patient may not think to volunteer their issue, making it important to proactively ask about how their eyes feel when they wear their mask. ECPs can provide simple advice about improving the mask seal along its top edge, taking breaks from drying tasks such as digital device use and the use of lubricating drops. Advice which has been summarized in an infographic available in over thirty languages from the Centre for Ocular Research & Education (CORE) (Figure 2). In existing CL wearers these discussions also provide a good reason to reassess lens comfort from other angles too. ECPs can re-evaluate the suitability of the lens material and modality being worn, and the condition of the ocular surface, lid margins and tear film. Some patients may benefit from a material change, a modality change to the flexibility of daily disposable lenses, an alternative lens care product, or therapy for ocular conditions such as blepharitis or meibomian gland dysfunction.
Dual wear
It is important to remember that the conversation around vision correction should not be framed as “either spectacles or CLs”. All CL wearers should have back up spectacles, but more than that, the majority of lens wearers actually identify as being dual wearers of both.2 This is a positive outcome for both the patient and ECP. The patient benefits from choice and flexibility of vision correction type depending on the task and situation; the ECP gains the opportunity to increase sales through spectacles, CLs, and ideally sunglasses too. An important point for ECPs is the repeat income CL sales can generate, a fact illustrated by their resilience of sales during the acute phase of lockdown in 2020, where 50%+ of all optical sales in 35% of practices were for CLs.21 The well-known “Enhancing the Approach to Selecting Eyewear (EASE)” UK-based study illustrates the dual benefits of CLs and spectacles perfectly.6 In the study, CLs were offered to patients to help them see themselves more clearly when selecting new spectacle frames. This approach removed the pressure of making the patient decide ahead of trying them whether they wanted to be a CL wearer. There was no initial choice to be made. Instead, they happened to experience CL wear while busy completing another task. The results showed positive impact all round. Spectacle dispensing value increased by 32%, more than three times the number of patients purchased CLs compared to the control (17 vs 5), and patients reported a superior spectacle dispensing experience.6 A similar approach conducted in the US also recorded positive results. Patients wearing CLs spent significantly more on their spectacles, were more than 2.5 times more likely to have received or scheduled a CL fit, and 93% reported that they were highly satisfied with the experience.7
A final, important point
The initial UK-based survey discussed in this article was prompted by realization that little growth exists in the number of CL wearers. In part, this can be addressed by following the advice outlined above: to commit to proactive recommendation with relevant language, and to offer more lens-on-eye experiences. However, it is worth mentioning one other aspect of CL growth and that is the subject of drop out. While a detailed examination of drop out is beyond the scope of the article, a few key points are worth highlighting to ensure new wearers have the best chance of continued success.
Firstly, the trial experience needs to be considered; a UK study (2019) with over 500 consumers who had recently experienced a CL trial concluded that 44% did not go on the purchase lenses.22 Just 20% were satisfied with their trial experience, compared to 83% of those who did become lens wearers (“convertors”). The good news, however, is that the negative experiences of the “non-converters” were driven by actions that could be relatively easily addressed by practice teams. Only 56% were satisfied with their application and removal teach training (versus 87% for converters) and 47% with the level of follow up from their ECP during the trial (versus 83% for converters). In addition, neophytes who had a more positive attitude to the future prospect of wearing CLs were more likely to convert to purchase. 26% of convertors wanted to try a different look to wearing their spectacles (compared to 19% for non-converters) and 12% said they wanted to trial because spectacles restrict them playing sport/exercising (versus 4% for non-converters). Converters had more notable engagement from the offset with 25% being curious to see what it would be like to trial contact lenses (compared to 17% for converters).
Additionally, in a prospective study of new CL fits, the retention rate was 77.6% (194/250) after twelve months, with the most common reason for discontinuation given as problems with vision (41%), followed by discomfort (36%) and handling problems (25%).
Conclusion
While it is easy to appreciate the practical benefits of wearing CLs, such as providing an alternative look, and removing restrictions on peripheral field of view, it is a little more challenging to truly appreciate how CLs affect the way people feel. The insights gained from thousands of CL wearers highlight deep and wide-ranging emotional benefits, including improved self-confidence and improved quality of life. It is important for everyone involved in eyecare to recognise these positive effects. Much more than a form of vision correction, CLs make the wearer feel different. ECPs are the gatekeeper for access to CLs, with the majority of patients looking for their practitioner to make a recommendation based on their suitability. What a great position for the ECP to hold: to be able to open those gates a little wider, tailoring the potential benefit to each patient, and proactively recommending CLs, alongside dual use of spectacles, to give many more patients the chance to see how they make them feel!
ACKNOWLEDGEMENT
This article is based on one first published in the Optician journal, UK in February 2021. Patel K et al. Contact lenses: so much more than simple correction of refractive error. Optician 2021; 15 Jan: 25-29
References
1. CVI data on file 2019. Industry and Market data, US consumer CL market in 2018.
2. Draper M, Patel K, Russell N. Mixed-methods study of behaviours and attitudes to vision correction of spectacle and contact lens wearers. Contact Lens and Anterior Eye 2019;42:e23.
3. Jones L, Jones D, Langley C, et al. Reactive or proactive contact lens fitting - does it make a difference? J Brit Contact Lens Assoc 1996;19:41-3.
4. Meyler J. STAR performers. Optician 1996;212:18-9.
5. Morgan S, Efron N. The benefits of a proactive approach to contact lens fitting. J BCLA 1996;19:97-101.
6. Atkins NP, Morgan SL, Morgan PB. Enhancing the approach to selecting eyewear (EASE): a multi-centre, practice-based study into the effect of applying contact lenses prior to spectacle dispensing. Contact lens & anterior eye 2009;32:103-7.
7. Mayers M, Jansen Bishop M, Walerius D, et al. Improving your spectacle patients' in-practice experience with contact lenses during frame selection. Contact lens & anterior eye 2019;42:406-10.
8. Lohr KN, Zebrack BJ. Using patient-reported outcomes in clinical practice: challenges and opportunities. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation 2009;18:99-107.
9. Kandel H, Khadka J, Goggin M, et al. Impact of refractive error on quality of life: a qualitative study. Clinical & experimental ophthalmology 2017;45:677-88.
10. Walline JJ, Jones LA, Sinnott L, et al. Randomized trial of the effect of contact lens wear on self-perception in children. Optometry and vision science 2009;86:222-32.
11. Rah MJ, Walline JJ, Jones-Jordan LA, et al. Vision specific quality of life of pediatric contact lens wearers. Optometry and vision science 2010;87:560-6.
12. Plowright AJ, Maldonado-Codina C, Howarth GF, et al. Daily disposable contact lenses versus spectacles in teenagers. Optometry and vision science 2015;92:44-52.
13. CVI data on file 2018. YouGov online survey on silicone hydrogel lenses. N=1520 adult CL wearers (US 519, UK 501, Japan 500). .
14. CVI data on file 2020. YouGov online consumer survey Nov/Dec 2019 in Germany, UK, Spain, Japan, USA. N=5,117 contact lens wearers ('consumers'), screened from total N=35.397 adults. Data weighted and representative of adults in each market (aged 18+).
15. CVI data on file 2020. Kubic online survey; n=404 US ODs who prescribe toric soft CLs.
16. Mintel report: optical goods retailing UK. Feb 2020; 2020.
17. CVI data on file 2020. COVID-19 spectacle wearers online survey, Verve, October 2020 Total n=1050, UK, Italy, Spain, Sweden, Germany, France, Poland.
18. CVI data on file 2020. YouGov online survey. 8,203 adults aged 18+ in US, Japan, Great Britain, Italy, Sweden, Canada, The Netherlands and Australia who wear glasses only (n=4,139) or both glasses and CLs (n=4,064). Fieldwork October 2020.
19. Moshirfar M, West WB, Marx DP. Face Mask-Associated Ocular Irritation and Dryness. Ophthalmology and Therapy 2020;9:397-400.
20. Jones L. Why face masks can make eyes feel dry, and what you can do about it. The Conversation; 2020 [updated 2020. Available at: https://theconversation.com/why-face-masks-can-make-eyes-feel-dry-and-what-you-can-do-about-it-143261. Accessed: 21 Oct 2020];
21. CVI data on file 2020. Covid-19 contact lens practitioner survey, Flame Health & Verve, May 2020. Base (all respondents): Total n=202 UK.
22. CVI data on file 2020. Covid-19 contact lens practitioner survey, Flame Health & Verve, May 2020. Base (all respondents): Total n=202 UK
22. Sulley A, Young G, Hunt C, et al. Retention Rates in New Contact Lens Wearers. Eye & contact lens 2018;44 Suppl 1:S273-S82.
24. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Contact lens & anterior eye 2017;40:15-24.
25. Maldonado-Codina C, Navascues Cornago M, Read M et al. The association of comfort and vision in soft toric contact lens wear. Contact Lens and Anterior Eye, 2020; In press








