2020 has delivered so many new and unexpected experiences. One of which is the need to wear face masks in public. For some people this may result in wearing a mask for just a few minutes a week while getting groceries. For others, such as healthcare workers and those in the service industry, it may mean wearing masks for extended periods of time throughout the day. This new, and necessary, experience brings with it some unhelpful side affects related to vision and ocular comfort. For these issues, the eye care practitioner is well placed to identify and advise their patients on what they can do to try and minimise the problem. Taking action is important not only to help patients feel more comfortable, but also to avoid them feeling discouraged about wearing masks in situations where they are required.
There are two eye-related issues: fogging of spectacle lenses and dry, uncomfortable feeling eyes.1 The former can happen the moment the mask is put on, affecting vision for the wearer. Dryness may occur in those people needing to wear masks for longer periods, resulting in worsening of symptoms in someone who already has dry eye disease, or creating uncomfortable eyes for the first time in someone who has not experienced dryness before.
The cause
The same process causes both spectacle fogging and dry-feeling eyes. While face masks do a good job of reducing the spread of airborne particles from the mouth and nose, they are of course not air tight. Exhaled air has to disperse somewhere, and it is this movement of air upon breathing out which causes the problems. Where the top edge of the face mask is not sitting snugly against the face, exhaled air is forced up and out of the top of the mask. The upward flow of warm air settles as condensation on spectacle lenses; the resulting fogging can significantly affect vision with each breath. Consistent movement of air over the ocular surface promotes increased evaporation of the tear film. Over a period of time, the resulting thinner and less stable tear film can lead to drying of the ocular surface.1 Clinically, increased ocular surface staining may be seen.1 Subjectively, the mask-wearer may report irritated, uncomfortable, red, dry-feeling eyes.1
Addressing spectacle lens fogging
Although it is not easy to eliminate fogging completely, there are a number of pieces of advice eye care practitioners can pass on to their patients. The fit of the face mask is a good place to start. Ideally, it should follow the contours of the nose and face closely along the top edge in order to discourage the upward movement of exhaled air. This may be achieved by repositioning the mask, trying a different design or shaped mask, or carefully taping the top edge with surgical tape to create a better seal. Spectacle position is important to address too. If the spectacle frames allow, then having it rest on top and in front of the mask can reduce airflow and fogging issues (Figure 1). It has been reported that washing spectacle lenses with soap and water can reduce fogging,2 although care must be exercised with this advice as not all lens coatings may be compatible with household soap. Perhaps a better option is to recommend use of a proprietary anti-fogging wipe or spray. Some patients may prefer to switch to, or even try for the first time, contact lenses to completely avoid the issue of fogging.

Figure 1: a) Fogging of spectacles while wearing a face mask;
b) Improved position of face mask and spectacles to reduce fogging.
(Images courtesy of Chau-Minh Phan, CORE, University of Waterloo).
Addressing ocular dryness
First coined by an Ophthalmologist in the US, this particular sequelae has been termed mask associated dry eye, or ‘MADE’.3 To reduce its occurrence, the first step is to follow the advice outlined above on achieving a good fit with the face mask, particularly along its top edge. The movement of air over the ocular surface creates a drying environment, so additional advice for this group of patients relates to balancing their exposure to other drying situations whilst wearing their mask. This might mean advice to take visual breaks from looking at digital devices more frequently when the mask is on, and trying to limit time in air conditioned environments where possible. Given that these environmental changes may not be possible for some, eye care practitioners may also wish to advise on the use of suitable artificial tear drops to help alleviate symptoms. All of these tips are available in an infographic to share with patients from the Centre for Ocular Research & Education (CORE) COVIDEyeFacts.org resource centre (Figure 2).
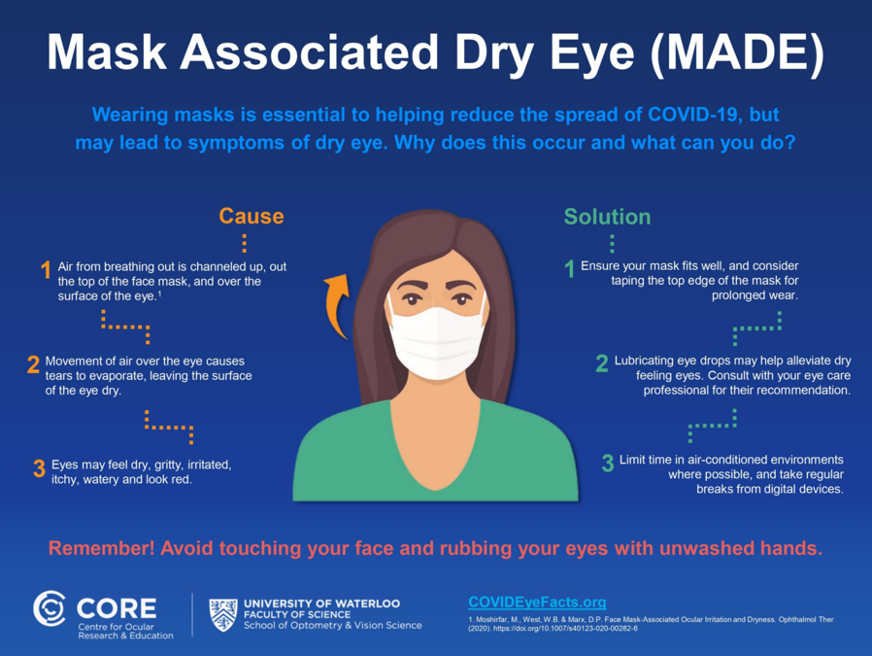
Figure 2: For use with patients to explain why MADE occurs and how to alleviate it
Be proactive
The simple advice outlined above could make all the difference to someone who is struggling to maintain mask wearing because of fogging or drying issues. Eye care practitioners are perfectly placed to identify the problem and pass on the tips to help minimise it. In particular for MADE the practitioner may wish to add in a proactive question to history and symptoms enquiring about ocular comfort when masks are worn.
___________________________________________________________________________________________________________
References
1. Moshirfar M, West WB, Marx DP. Face Mask-Associated Ocular Irritation and Dryness. Ophthalmology and Therapy 2020;9:397-400.
2. Malik SS, Malik SS. A simple method to prevent spectacle lenses misting up on wearing a face mask. Annals of the Royal College of Surgeons of England 2011;93:168-.
3. Jones L. Why face masks can make eyes feel dry, and what you can do about it. The Conversation; 2020 [updated 2020. Available at: https://theconversation.com/why-face-masks-can-make-eyes-feel-dry-and-what-you-can-do-about-it-143261. Accessed: 21 Oct 2020];








