The second part in a series, this article discusses the opportunities in toric lens fitting and care. Click here to read part 1.
The wide variation in soft toric fitting practices around the world, coupled with a sense that some ECPs are not fully confident in the ease of fitting and overall performance of soft torics provides a number of areas to address. Discussed below, these relate to broad areas such as patient needs, professional communication, product performance, and practice set up. Addressing these concerns should help support ECPs who do not already embrace soft toric options to feel more confident in recommending them more frequently.
The importance of correcting low levels of astigmatism
Low to moderate levels of astigmatism are rarely omitted from spectacle corrections. Leaving 1.00D of astigmatism uncorrected can result in a significant decrease in distance and near visual acuity,20 reading speed,20 decrease reading fluency,21 and stereoacuity.22 Symptoms of ocular discomfort, dry eye and headaches can also result from uncorrected astigmatism.20,21 A once popularly held view that thick or high modulus spherical designs can ‘mask’ astigmatism has proved not to be true.23-26 Likewise, aspheric lenses do not demonstrate improved visual outcomes for low astigmats compared to toric corrections.27,28
The link between comfort and vision in soft toric lens wear35
Poor satisfaction with vision in contact lenses is clearly undesirable and can ultimately lead to drop out. Sub-optimal vision performance is a significant cause of contact lens drop out by itself.29,30 Astigmats have been shown to over-index in contact lens drop outs, 29,31,32 a fact which serves as a reminder to ensure the vision and comfort needs of this patient group are fully met in contact lenses.
When compared with spherical lenses, correction of astigmats with toric lens designs results in significantly improved subjective and objective visual performance.36,37 This can be demonstrated to a patient in practice by having them view the smallest line of letters they can see both with and without the cylinder correction in place. These differences can be subtle and are often better demonstrated using a real-world target. The benefit could be demonstrated via viewing small detail on digital devices, or with night driving for instance. If an extended trial is not practical or desired, ensuring examples of real-world visual tasks are available to view in practice is a good alternative.
Patient expectations
Sub-optimal vision or comfort can result in drop out from lens wear. For new wearers, a prospective study established the drop out at twelve months to be 22.4%, with poor vision being cited as the main cause of discontinuation (41%) followed by comfort (36%).32 This highlights once again the importance of ensuring a patient is happy with the comfort and vision in their contact lenses.
Recent insights have generated a better picture of the expectations that patients place on their ECP too. Health and vision are both in the minds of patients when considering what they want to hear from their ECP. A survey of more than 5,000 lens wearers in five countries established that 86% agree they expect their ECP to make a recommendation for the soft contact lenses that provide the best possible vision correction for their eyes, regardless of cost.39 The fact that patients expect to hear about their best options regardless of cost is noteworthy. This information should help overcome any barrier in the ECP’s mind about price. The message from the patient is clear: “tell me about the best options to help me make an informed choice.”
Product performance and practice set up
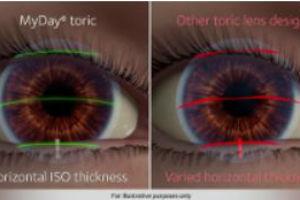
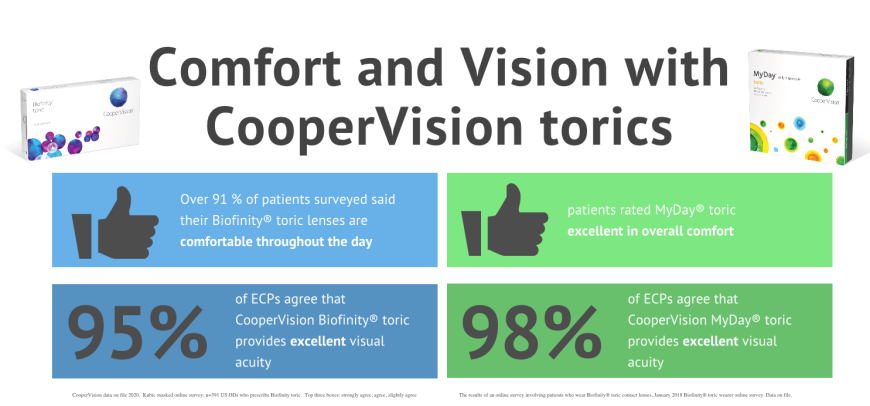
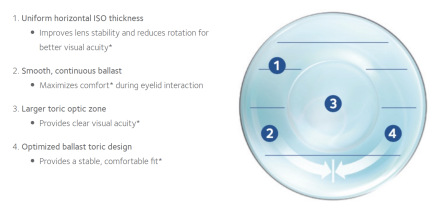
The performance of early hydrogel soft toric designs include reports of intolerance, inadequate fit, handling difficulties and problems with vision.40 Unpredictable fitting characteristics,41 and variable lens position with blinking,42 and head position,2,3 all contribute to fluctuating vision and poor outcomes. Given this history, it is understandable, that some ECPs may still hold concerns about the performance of soft toric lenses.8 However, the design of modern toric lenses has evolved over time, with currently available options designed to achieve both quick and consistent fitting for the ECP, along with delivering comfort and stable vision for the wearer. Optimized Toric Lens Geometry™, found in both Biofinity® toric and MyDay® toric contact lenses provides excellent stability for an optimal toric lens wearing exprience.
Several studies have examined the performance of these designs for static high contrast acuity, real-world visual tasks, rotational stability with eye and head movements, and rotational recovery, generally reporting, with some small differences between designs, that modern methods of stabilization perform well.2-7 In fact, a recent analysis of over four hundred subjects from ten clinical trials using one proprietary design established across a number of factors, that a successful lens experience was achieved in all categories 83% of the time.43 Those factors included orientation success, fit acceptance, visual acuity, visual quality and comfort, and each individually returned success over 90% of the time.43
Successful fitting of astigmats in three different groups has been demonstrated: existing soft spherical lens wearers, contact lens drop outs and neophytes.44 In order, the fit success rate for those three groups was 80%, 75% and 70%, with previous spherical lens wearers also recording an improvement in visual acuity, and the neophyte group a level of vision in their contacts lenses comparable to their spectacles. Results such as this should help build confidence in the visual performance of soft torics compared to spectacles.
Limited prescription availability is a barrier sometime cited by ECPs. It is of interest to note ECPs tend to underestimate the proportion of patients that can be corrected with available soft toric contact lenses. When asked in a recent survey, ECPs felt one single reusable soft toric on average could be prescribed to between 55-74% of their patients depending on the product.8 When modern soft toric lens availability was compared to a large database of spectacle prescriptions it was actually shown that typical coverage is higher than ECPs believe. An example of this is a toric lens with cylinder correction available up to -1.75D, spherical powers from +4.00D to -8.00D and 10 degree axes available around the clock actually provides cover for at least 90% of spectacle prescriptions,45 and this would be even higher for some soft toric lenses that have additional parameters available.
The length of time required to achieve a successful soft toric fit has been voiced as a concern in the past. Modern soft toric lenses are actually as quick to fit as spherical lenses,1 the fitting of which can be further supported by manufacturer supplied fitting sets and online fitting calculators. Both of these enable time-efficient fitting for ECPs and patients.
Initial lens selection, either from the trial set or via pre-ordering, can be supported in a number of ways. This may be via printed manufacturer fit guides and tools which confirm available prescription range, through to online toric lens calculators available, such as the OptiExpert® app. Accuracy of OptiExpert® has been shown to agree with investigator prescribed final prescriptions in 9 out of 10 eyes for different toric lenses.46,47 Use of OptiExpert® supports accurate initial trial lens selection for the brand of toric lenses in question, and also enables trained support staff to order trial lenses in ahead of scheduled-appointments if required. Both the accuracy of initial prescription choice, and the ability to use staff to order ahead, are helpful to ensure efficient use of time in practice. These approaches can be applied to other lens fittings, including spherical and multifocal.
Where might other opportunitis to build upon toric success exist? Click here for Part 3 in this series, Additional Opportunities
________________________________________________________________
REFERENCES
20. Wolffsohn JS, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. Journal of cataract and refractive surgery 2011;37:454-60.
21. Wills J, Gillett R, Eastwell E, et al. Effect of simulated astigmatic refractive error on reading performance in the young. Optometry and vision science 2012;89:271-6.
22. Al-Qahtani H, Al-Debasi H. The effects of experimentally induced graded monocular and binocular astigmatism on near stereoacuity. Saudi Journal of Ophthalmology 2018;32:275-9.
23. Bernstein P, Gundel R, Rosen J. Masking corneal toricity with hydrogels: does it work? Int Contact Lens Clin 1991;18:67-70.
24. Snyder C, Talley DK. Masking of astigmatism with selected spherical soft contact lenses. Journal of the American Optometric Association 1989;60:728-31.
25. Edmonson LL, Edmondson W, Price R. Masking astigmatism Ciba Focus Night & Day vs Focus Monthly. Optometry and vision science 2003;80 (supp) 184.
26. Cho P, Woo GC. Vision of low astigmats through thick and thin lathe-cut soft contact lenses. Contact lens & anterior eye 2001;24:153-60.
27. Kollbaum PS, Bradley A. Aspheric contact lenses: Fact and fiction. Contact Lens Spectrum 2005;20:34 - 8.
28. Morgan PB, Efron SE, Efron N, et al. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optometry and vision science 2005;82:823-8.
29. Young G. Why one million contact lens wearers dropped out. Contact lens & anterior eye 2004;27:83-5.
30. Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Contact lens & anterior eye 2017;40:15-24.
31. Young G, Veys J, Pritchard N, et al. A multi-centre study of lapsed contact lens wearers. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians 2002;22:516-27.
32. Sulley A, Young G, Hunt C, et al. Retention Rates in New Contact Lens Wearers. Eye & contact lens 2018;44 Suppl 1:S273-S82.
33. Rao SB, Simpson TL. Influence of Vision on Ocular Comfort Ratings. Optometry and vision science 2016;93:793-800.
34. Orsborn G, Vega J, Orsborn G. Correlation Between Ocular Comfort and Vision Quality of Three Daily Disposable Soft Toric Contact Lenses with Different Moduli of Elasticity. Contact Lens and Anterior Eye 2019;42:e12.
35. Maldonado-Codina C, Navascues Cornago M, Read ML, et al. The association of comfort and vision in soft toric contact lens wear. Contact Lens and Anterior Eye 2020.
36. Cho P, Cheung SW, Charm J. Visual outcome of Soflens Daily Disposable and Soflens Daily Disposable for Astigmatism in subjects with low astigmatism. Clinical & experimental optometry 2012;95:43-7.
37. Kruse A, Lofstrom T. How much visual benefit does an astigmat achieve being corrected with a toric correction? Int Contact Lens Clin 1996;23:59-65.
38. CVI data on file 2018. YouGov online survey on silicone hydrogel lenses. N=1520 adult CL wearers (US 519, UK 501, Japan 500). .
39. CVI data on file 2020. Contact lens consumer confidence online survey, conducted Nov-Dec 2019 by YouGov Plc. Total of 5,347 contact lens wearers in 5 countries (Germany, Great Britain, Japan, Spain and the US).
40. Evans J, Hau S. The therapeutic and optical application of a rigid gas permeable semi-limbal diameter contact lens. Contact lens & anterior eye 2009;32:165-9.
41. Tan J, Papas E, Carnt N, et al. Performance standards for toric soft contact lenses. Optometry and vision science 2007;84:422-8.
42. Tomlinson A, Ridder W, Watanabe R. Blink-induced variations in visual performance with toric soft contact lenses. Optometry and vision science 1994;71:545-9.
43. Sulley A & Greenaway N. Success rates with a toric soft contact lens design. Optom Vis Sci 2020;97(E-abstract):205296.
44. Sulley A, Young G, Lorenz KO, et al. Clinical evaluation of fitting toric soft contact lenses to current non-users. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians 2013;33:94-103.
45. Luensmann D, Schaeffer JL, Rumney NJ, et al. Spectacle prescriptions review to determine prevalence of ametropia and coverage of frequent replacement soft toric contact lenses. Contact Lens and Anterior Eye 2018;41.
46. Luensmann D, Woods J, Patel S. Validation of an online lens fitting app for two daily disposable toric lenses. Contact Lens and Anterior Eye 2019;42:e38-e9.
47. Luensmann D, Woods J, McParland M. Toric lens fitting success supported by an online fitting App. In: NCC. Eindhoven; 2020.