Today’s soft toric contact lenses have evolved considerably since the first lens in this category, the Hyrdocurve Soft Toric, gained FDA approval in 1978.1,2 Early designs were generally thick, comprised of low-water content, and unreliable, which often led to fitting concerns when it came to vision, orientation, stability, and comfort.2,3
Modern soft toric designs are significantly different from their early counterparts, with improved overall performance in ease of fit, comfort, rotational stability, and vision, all of which provide successful fitting opportunities for eye care professionals (ECPs) and for a wide range of their astigmatic patients.4
Case in point: Recent studies have suggested that patients with astigmatism who are new wearers or previous contact lens dropouts achieve visual acuity comparable to spectacles when fitted with modern toric designs.5
Dr. Dave Anderson, OD, of Miamisburg Vision Care in Miamisburg, Ohio, shares how today’s modern toric lenses seamlessly fit into ECPs’ day-to-day practice and how CooperVision’s soft toric contact lens options are his go-to in his toric treatment toolbox.
Can you share how overall innovations and new technology in toric lenses have changed in recent years, and in doing so, improved patients’ vision and wearing experience?
Over the years, so many different designs and increased parameters have made fitting toric lenses much easier. I generally have an option for every patient who has a desire to wear contact lenses. In years past, toric lenses were often uncomfortable, unstable, and only came in small ranges. I would occasionally shy away from fitting someone because of these challenges, but today, I love that nearly any patient can have access to the freedom contact lenses provide. From mutifocal toric lenses to daily disposable lenses, I never consider someone’s prescription a barrier, and with the improved stability, the environment of a patient doesn’t change my thoughts on their ability to wear a lens.
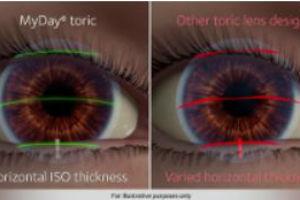
From your perspective, how has new technology, including Optimized Toric Lens Geometry®, helped your patients achieve a more stable, predictable, and comfortable fit, while also providing consistent visual acuity?

Optomized Toric Lens Geometry® allows for both a more stable and consistent lens wearing experience. In years past, a patient’s prescription could often create challenges in lens stability, vision, and overall comfort. With Optimized Toric Lens Geometry®, lenses are much more stable,*6 and even with subtle differences in lid shape or corneal curvature, I never shy away from an opportunity to give these lenses a chance on someone’s eyes. But for me, having a very large optic zone brings excellent vision.7 Most patients with astigmatism struggle to achieve optimal vision and have to tolerate approximation adjustments to their prescription or optics that aren’t ideal. Today’s Optimized Toric Lens Geometry® provides a larger optic zone and stable lens, creating a visual experience that allows me to tell glasses wearers that their vision will be the same with contacts, †8something I would have never said in the not too recent past.
CooperVision recently expanded its parameter range for MyDay® toric, increasing its current range by nearly 70% and matching the industry-leading range of Biofinity® toric.9Has MyDay® torics’ parameter expansion offered greater opportunities for your astigmatic patients? If so, can you provide an example?
The expanded parameters are such an exciting opportunity for me since this has allowed me to fit so many more patients. One specific patient of mine, who is now the director of HR at my practice, has struggled to wear contacts since shortly after I hired her. She wore a gas permeable contact for over 20 years, but her eyes became very dry since she stared at computers all day as part of her job. Because of this, she went from a full-time, 16-hour-a-day wearer to a weekend warrior to a full-time glasses wearer. We tried several standard soft lenses that were close to her prescription, but the vision wasn’t acceptable. She wanted a daily lens, and after eight different soft spherical lenses, we gave up and switched to scleral lenses. She did enjoy the vision and comfort of the sclerals but didn’t like all the work involved. She also felt it was too much of a hassle to take them on vacation or weekend trips to watch her son play baseball. She is a moderate hyperope with significant astigmatism and an oblique axis – so she was a challenging patient who still wanted to wear contacts, but there were so few options…. until now! At first, my employee was very hesitant to try them, assuming they would not work like others we tried over many years, but in an instant, she was so excited to have clear vision and said the MyDay® toric felt like nothing was on her eye.10,11
CooperVision’s OptiExpert® Contact Lens Calculator provides ECPs a tool to calculate the recommended diagnostic toric contact lens for their astigmatic patients.12 Do you use the OptiExpert® fitting app? If so, can you discuss your experience with it?
OptiExpert® is quite simple and quick to provide lens fitting options. ‡12,13 Most typically, I can do this in my head but having a quick and easy to-use tool does help me troubleshoot some difficult fits.
Can you share your approach when it comes to astigmatic contact lens wearers who’ve crossed over to presbyopia?
As patients age and begin noticing troubles at near, they don’t want to stop wearing contacts. Long before they have a need, I begin discussing options with them, and I always provide all options. I start my discussion with reading glasses, go over monovision and then discuss the major advantages of multifocals, namely the Biofinity® toric multifocal. I generally tell them, as we get closer to this need, it will be a seamless transition to help them see far and near while wearing a contact lens, similar to what they already wear. Having options that can solve these visual issues allow patients the option to wear contacts far past the time they begin to have near issues.
Finally, how do CooperVision’s toric contact lens options fit into a practitioner’s astigmatic contact lens toolbox?
Overall, all the options truly allow me to tell every patient that they are indeed a candidate for contact lenses.14 Just recently, a staff member who has been told for over 15 years that she could not wear contacts asked me if she was a contact lens candidate. I laughed at the thought that someone still thinks, just because they have astigmatism, their ECP can’t find a lens that would work for them. With huge parameter ranges and several materials and replacement modalities, CooperVision has an option for almost any patient.15 My new staff member tried a lens that day – and with tears welling up in her eyes, she said to me, “This is amazing. I’m so happy and can’t wait to tell all my friends that I can wear contacts!”