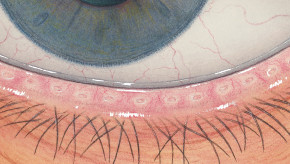
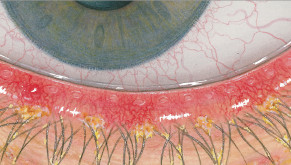
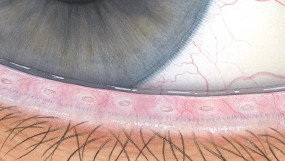
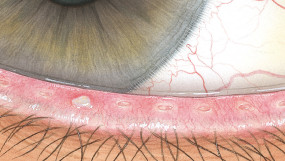
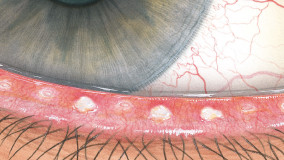
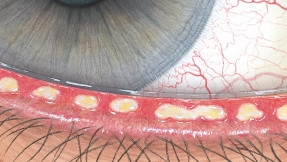
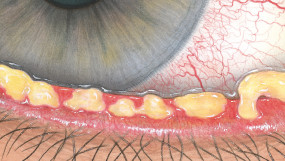
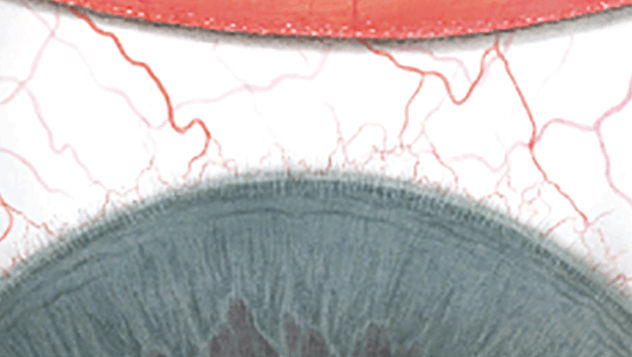
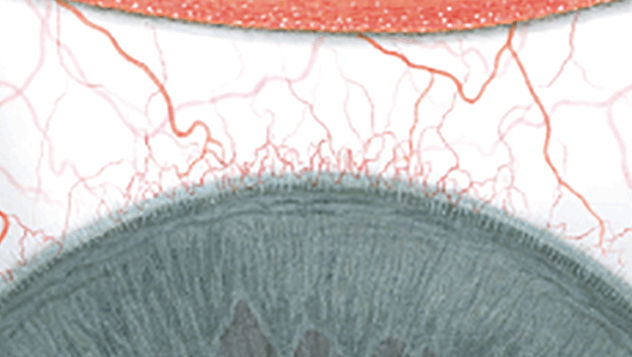
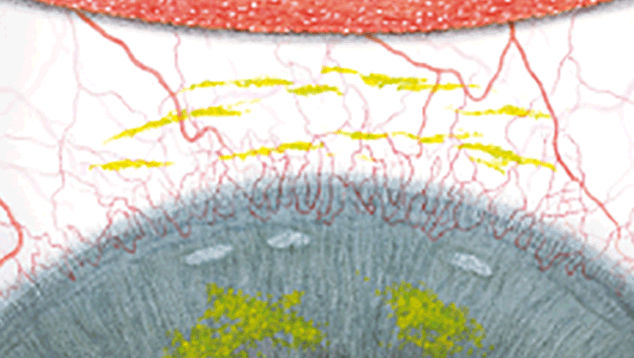
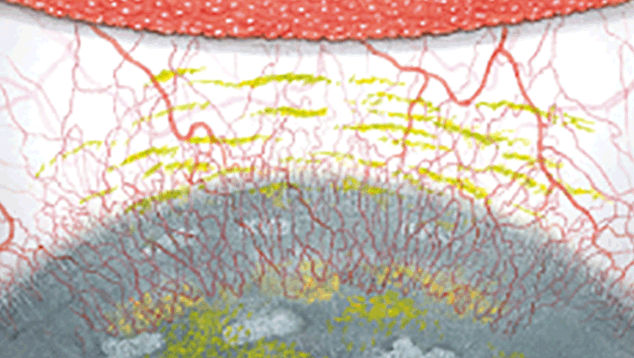
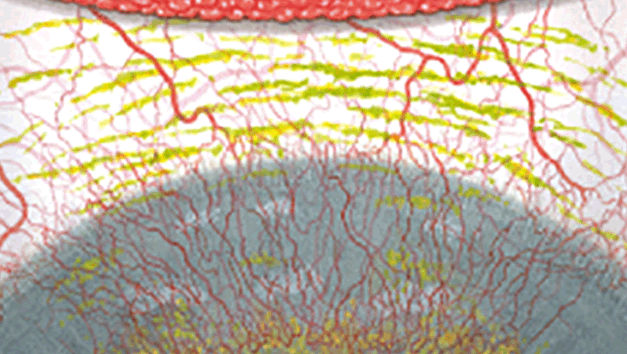
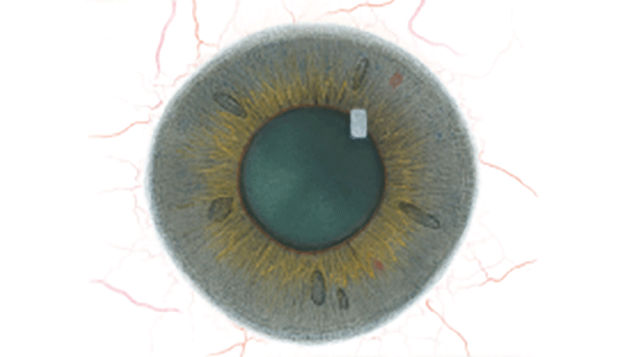
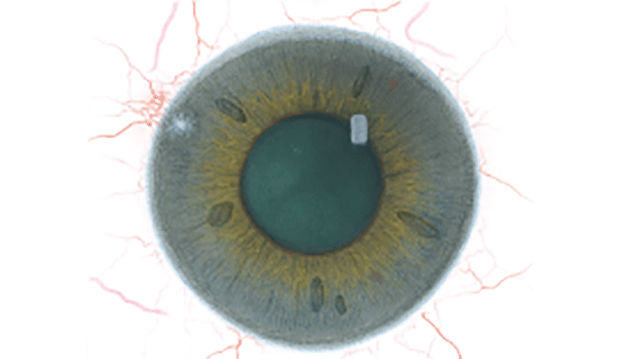
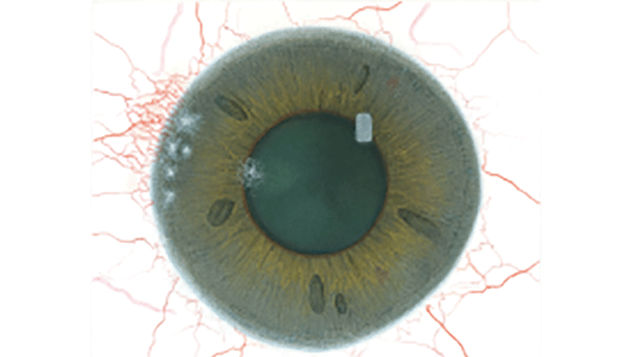
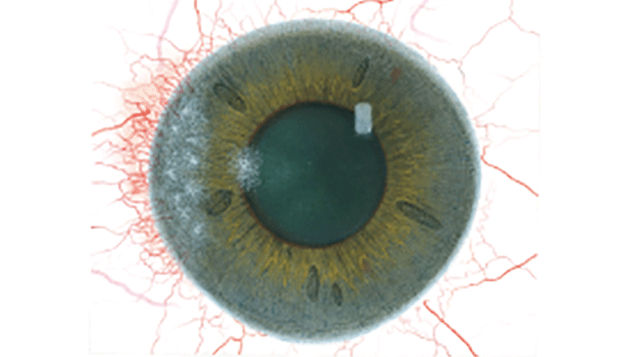
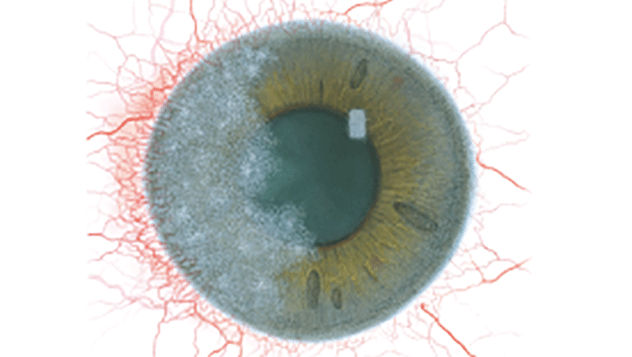
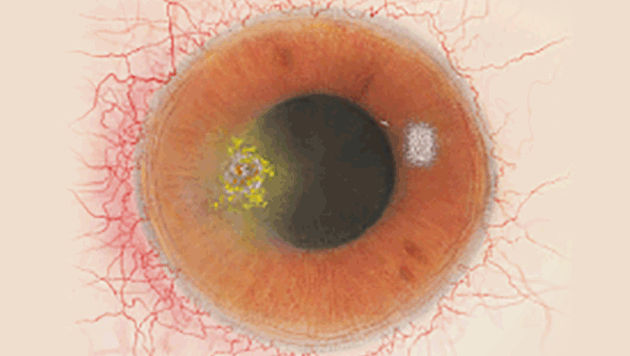
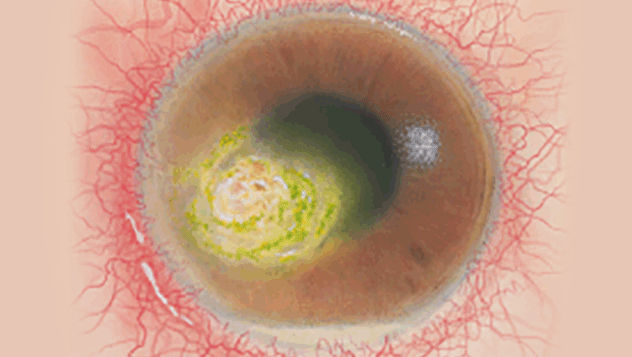
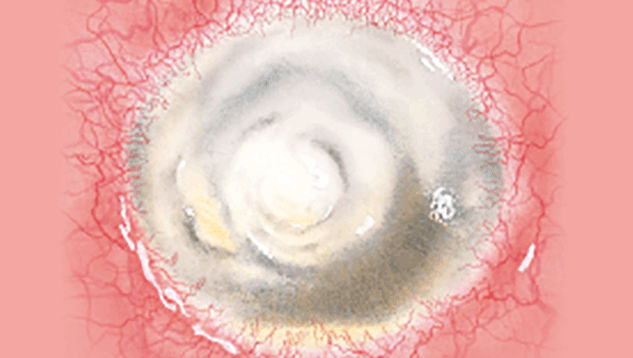
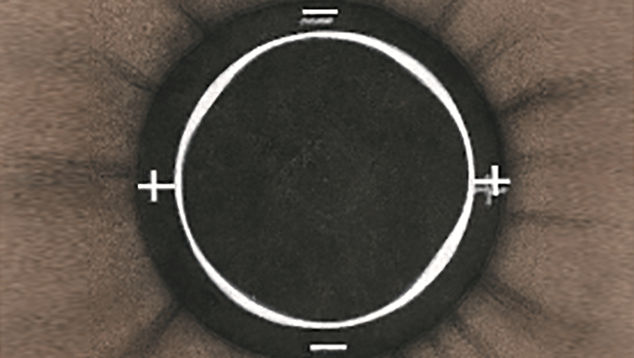
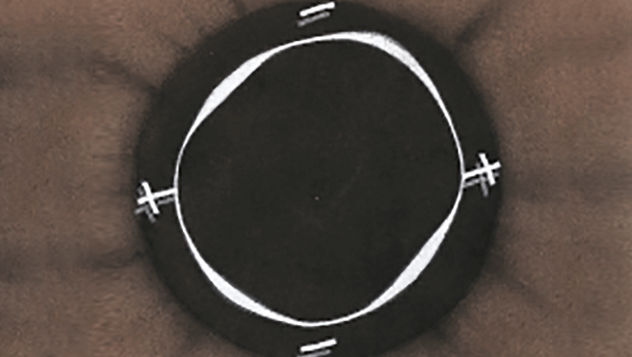
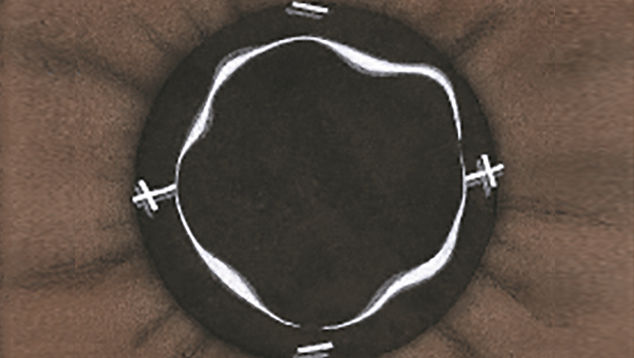
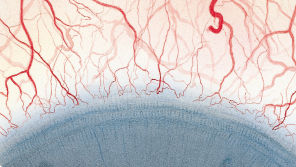
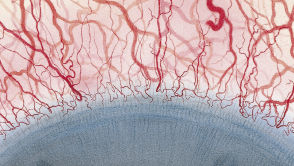
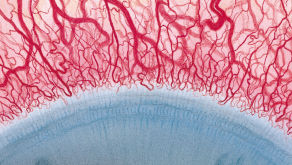
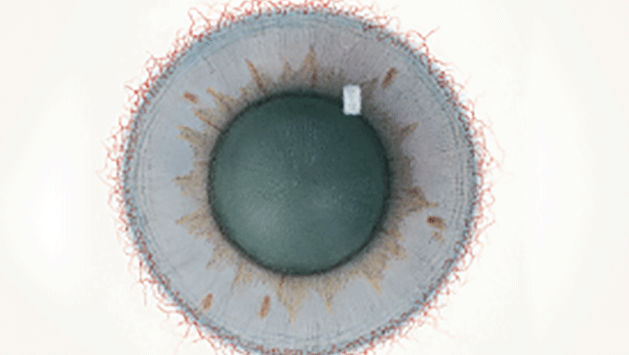
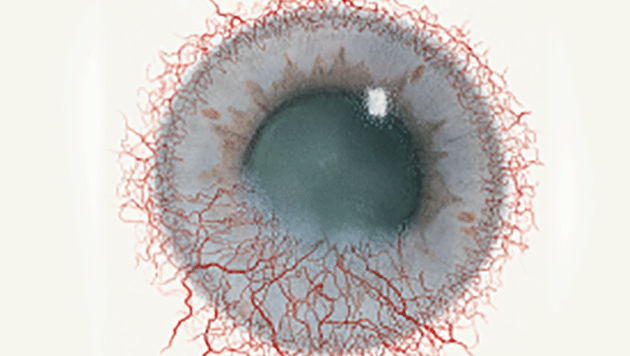
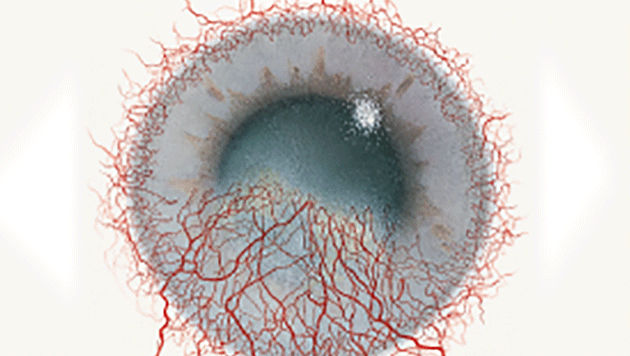
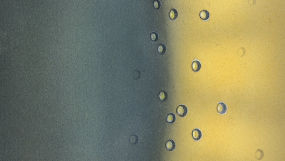
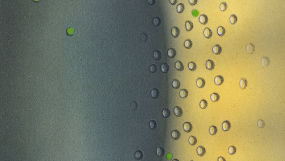
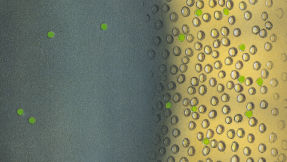
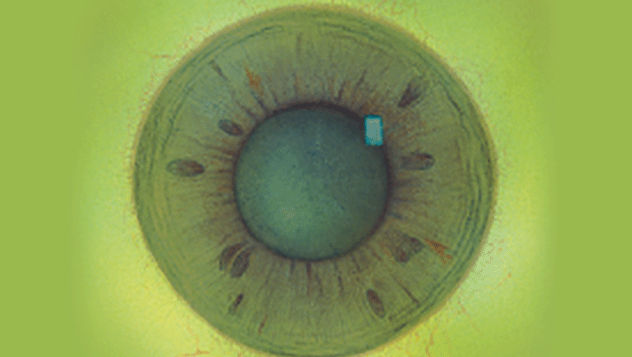
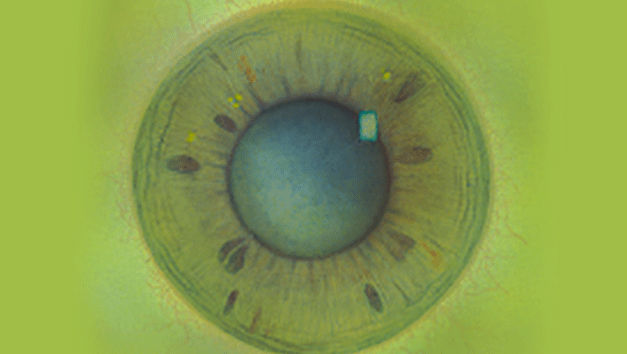
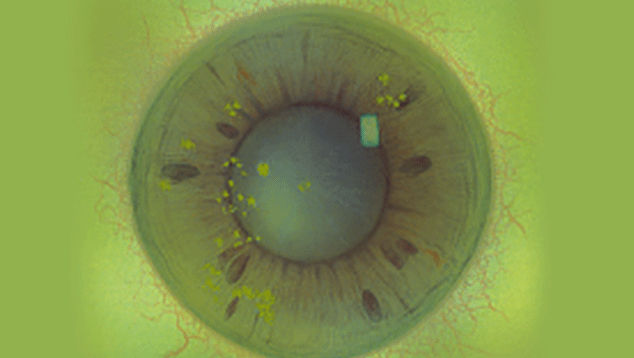
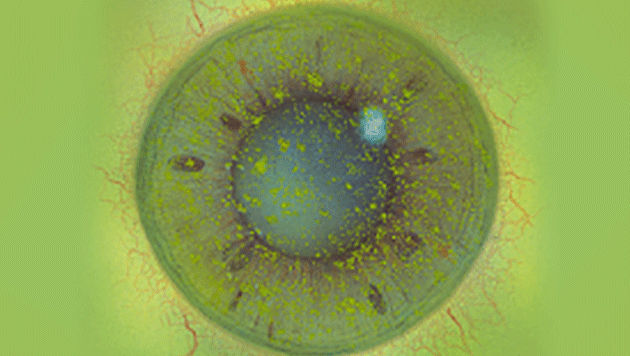
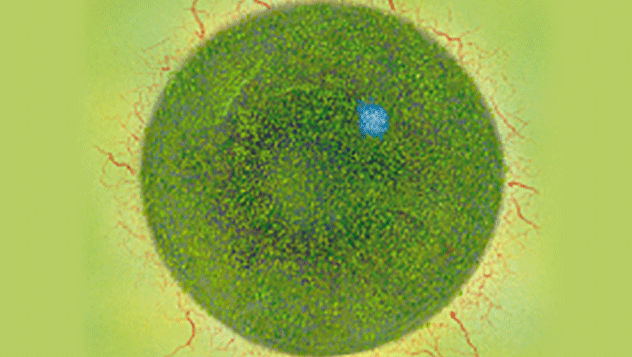
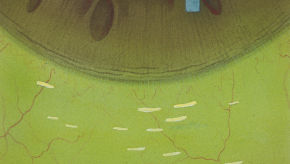
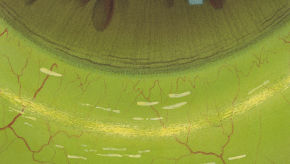
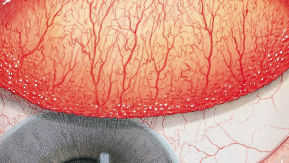
The Efron Grading Scales* provide a convenient clinical reference for eye care professionals. On a scale of 0 to 4, it describes the severity of the following anterior ocular complications that can occur from contact lens wear.
- Blepharitis
- Meibomian gland dysfunction
- Superior limbic keratoconjunctivitis
- Corneal infiltrates
- Corneal ulcer
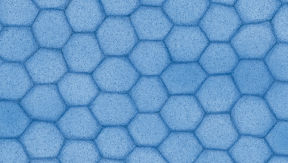
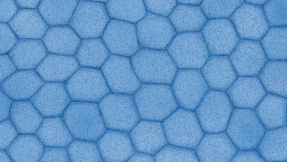
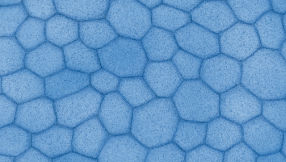
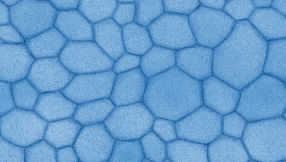
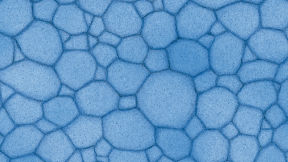
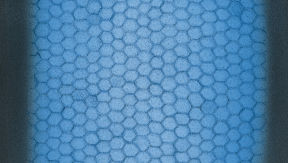
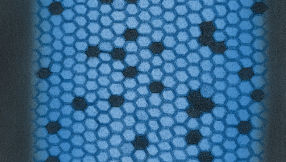
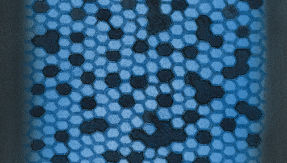
- Endothelial polymegethism
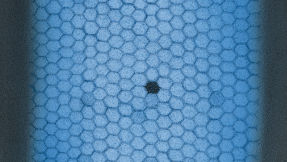
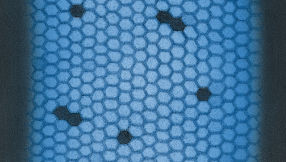
- Endothelial blebs
- Corneal distortion
- Conjunctival redness
- Limbal redness
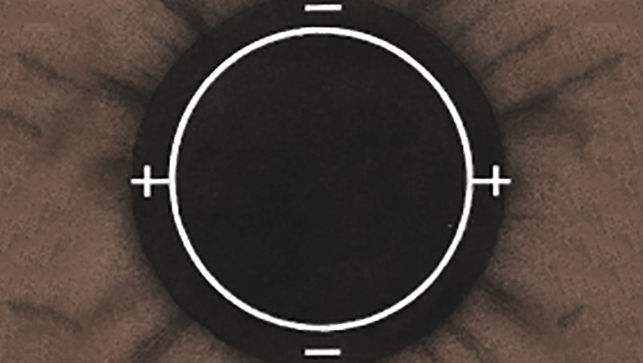
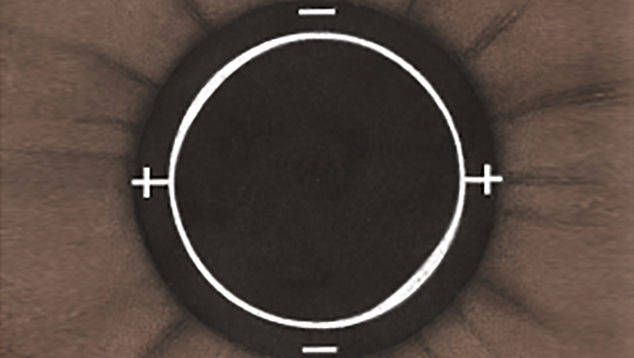
- Corneal neovascularisation
- Epithelial microcysts
- Corneal oedema
- Corneal staining
- Conjunctival staining
- Papillary conjunctivitis
Each condition includes five illustrations. Simply select a number on the scale for the corresponding illustration and visual signs of severity. Select the Info button for symptoms, pathology, treatment options and more.
* The calculator is designed to aid eye care practitioners. It is not a replacement for a professional consultation with a qualified eye care practitioner.